Americans aren’t getting any younger. This year, 2.5 million baby boomers will turn 70, according to the AARP, and the other 74.9 million living boomers are all over 50.
As this celebrated generation enters their golden years, the healthcare industry faces a challenging new reality: An aging patient population means more individuals with multiple chronic diseases and complex medical needs.
To keep at-risk patients healthy and healthcare costs down, many care providers are now investing in remote patient monitoring solutions.
Extra Attention for At-Risk Patients
Primary care providers (PCPs) are already overwhelmed with patient loads and paperwork, and many can’t see chronically ill patients as frequently as they need to be seen. These individuals are often redirected to urgent care clinics or hospital emergency rooms, even for minor problems. This results in higher costs for healthcare plans and readmission penalties for hospitals. It also disrupts the continuity of care for patients.
That’s why forward-thinking healthcare leaders are taking a more proactive approach to disease management. Two-thirds of hospitals and health systems have now deployed remote patient monitoring solutions, according to Spyglass Consulting. These solutions are typically managed by home health networks.
“Within the Medicare population, 20 percent of patients are considered ‘chronically frail,’ and they account for 80 percent of dollars spent,” explains Dr. Arta Bakshandeh, senior medical director for Alignment Healthcare (AHC), a population health management company serving high-risk medicare patients in California, North Carolina and Florida. “We take on the management of these patients, ensuring they get the extra attention they need. Then PCPs can focus on routine health maintenance for the 80 percent of patients we call ‘walking well.'”
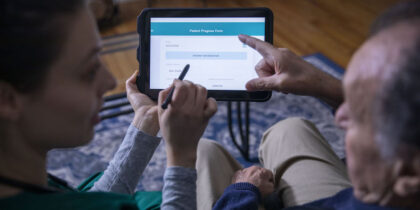
To do so, AHC built clinics where patients can see medical professionals as often as needed. For the patients Dr. Bakshandeh calls “the frailest of the frail,” AHC also uses Vivify Health’s remote care platform on Samsung Galaxy tablets.
Economic Benefits of Remote Patient Monitoring
More than 120 AHC patients use the Vivify/Samsung solution, with an 86 percent compliance rate. These patients receive ongoing disease management education, take more responsibility for their health and are far less likely to be admitted to the hospital. The remote care solution also offers them:
1. Continuity of Care
When chronically ill patients are bounced around from doctor to doctor, important information can get lost in the shuffle, leading to costly oversights and mishaps. “One of the greatest challenges in healthcare is fragmentation,” says Dr. Bakshandeh. “Physicians aren’t talking to each other. Pharmacies and hospitals aren’t talking to each other. The PCP doesn’t understand what happened to their patients, because they went to four different places.” With the Vivify platform, patient data is in one place and can easily be communicated to physicians.
2. Continuous Data
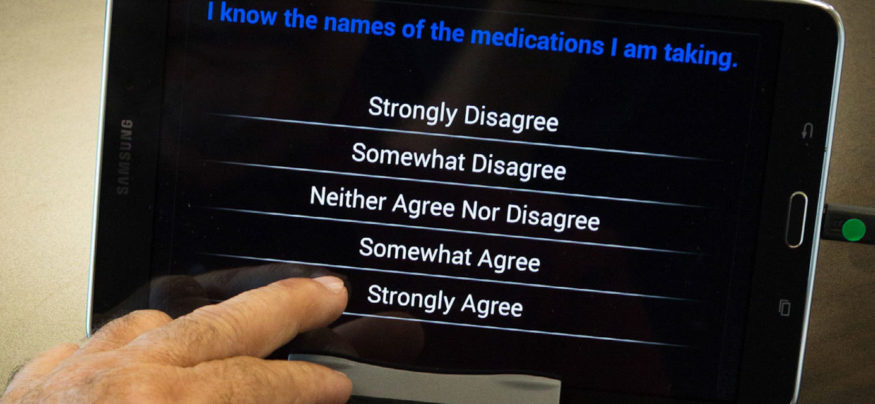
Each day, AHC’s remote care patients use Bluetooth-enabled medical devices — weight scales, blood pressure cuffs and oximeters — to capture biometric data on the Samsung tablet and transmit it to AHC’s Command Center. Patients also answer a series of daily questions based on their medical conditions and care plans.
3. Proactive Intervention
AHC’s team continuously monitors data and immediately follows up with patients when they spot troubling trends. For example, when Dr. Bakshandeh noticed a diabetic patient reporting low blood sugar, he called to find out why. The patient explained that he was afraid to eat, because he didn’t know what foods were safe. He was skipping meals but still taking his medications. “He said to me, ‘I don’t know who to talk to about it, but I’m so appreciative that you guys are watching me,'” recalls Dr. Bakshandeh. “After we hung up, I contacted our social worker, who arranged for this patient to receive diabetic meals on wheels. Without remote monitoring, no one would have known this patient’s problem until he saw a clinician or ended up in the ER.”
4. Virtual Patient Visits
Biometric data reveals a lot about patients’ conditions, but so does actually seeing those patients. For example, a video call with one patient helped a nurse practitioner to diagnose a gastrointestinal bleed. They transferred the patient to a local hospital, where she bypassed the ER and saw a gastroenterologist immediately.
“She had two units of blood transfused within the hour and was able to stay on a telemetry unit, rather than ICU,” says Dr. Bakshandeh. “This woman was on her way to stroke, heart attack and potentially death within 24 to 48 hours. It would have been a catastrophe — not only from her quality of life standpoint, but also from a financial standpoint. But because we had a simple face-to-face with her via video, we were able to diagnose her, address the issue, and get her back home with no deficits in less than two days.”
To learn more about Alignment Healthcare’s mission to improve patient outcomes, read the full case study.